Context:
A recent report by the Global Snakebite Taskforce (GST) highlights a major gap in India’s capacity to manage snakebite cases effectively. According to the survey, 99% of healthcare workers in India face challenges in administering antivenom—the life-saving therapy that neutralises venom toxins.
Background:
India accounts for nearly half of global snakebite deaths, with around 58,000 fatalities annually. Despite being the world’s largest producer and consumer of antivenoms, challenges such as delayed access to care, weak rural healthcare systems, and infrastructure gaps significantly hinder effective treatment. Snakebite envenoming remains a silent crisis, disproportionately affecting rural and agricultural communities, particularly during the monsoon season. Meanwhile, urban areas face rising risks due to rapid urbanisation and poor waste management.
Global and National Scenario:
-
-
-
- Globally, about 5.4 million people are bitten by snakes each year, with 1.8 to 2.7 million cases resulting in venom exposure. Annually, snakebites cause between 81,410 and 137,880 deaths worldwide, leaving many survivors with amputations or permanent disabilities. Recognising its severity, the World Health Organization (WHO) has classified snakebite envenoming as a high-priority neglected tropical disease.
- In India, the diversity of venomous snakes is remarkable, with over 300 species, more than 60 of which are venomous. The “Big Four”—the Indian cobra, common krait, Russell’s viper, and saw-scaled viper—account for most fatalities. A study covering the period from 2001 to 2014 estimated 1.2 million deaths and 3.6 million cases of permanent disability, implying that nearly one in 250 Indians faces a lifetime risk of dying from a snakebite.
- Globally, about 5.4 million people are bitten by snakes each year, with 1.8 to 2.7 million cases resulting in venom exposure. Annually, snakebites cause between 81,410 and 137,880 deaths worldwide, leaving many survivors with amputations or permanent disabilities. Recognising its severity, the World Health Organization (WHO) has classified snakebite envenoming as a high-priority neglected tropical disease.
-
-
About Antivenoms:
-
-
-
- Snake venom contains haemotoxins, neurotoxins, and cytotoxins that can destroy blood cells, paralyse nerves, and dissolve tissues. Antivenoms are life-saving medicines that bind to and neutralise venom toxins, enabling the immune system to eliminate them safely. India’s polyvalent antivenoms primarily target the Big Four but do not cover species such as king cobras or pit vipers.
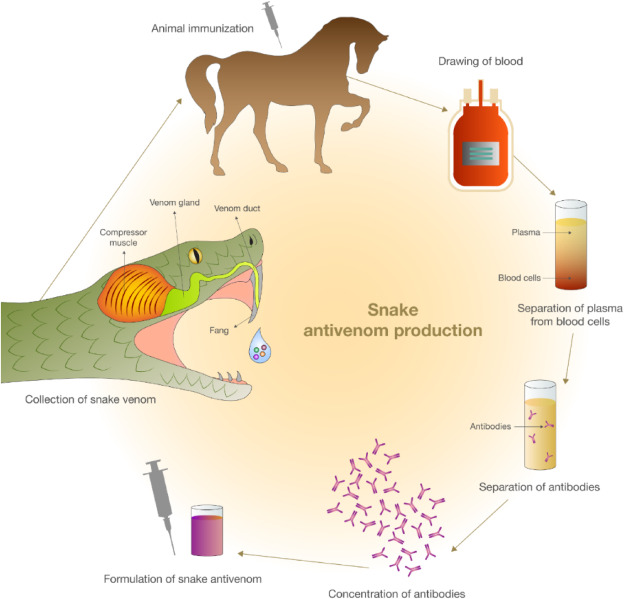
- Antivenom production involves milking venomous snakes, immunising animals (usually horses or sheep), and extracting antibodies. The Irula tribe of Tamil Nadu supplies nearly 80% of the venom used in antivenom production, operating under regulated permits in accordance with the Wildlife Protection Act, 1972.
- Snake venom contains haemotoxins, neurotoxins, and cytotoxins that can destroy blood cells, paralyse nerves, and dissolve tissues. Antivenoms are life-saving medicines that bind to and neutralise venom toxins, enabling the immune system to eliminate them safely. India’s polyvalent antivenoms primarily target the Big Four but do not cover species such as king cobras or pit vipers.
-
-
Challenges in Accessing Antivenoms:
-
-
-
- Despite domestic production, access to antivenoms faces multiple barriers:
- Geographical: Remote and rural areas lack nearby healthcare facilities.
- Cultural: Superstitions and traditional beliefs delay timely medical care.
- Economic: High production costs limit affordability and availability.
- Logistical: Inadequate cold-chain infrastructure degrades antivenom quality.
- Geographical: Remote and rural areas lack nearby healthcare facilities.
- These challenges result in delayed treatment, severe complications, and preventable deaths.
- Despite domestic production, access to antivenoms faces multiple barriers:
-
-
Way Forward:
Reducing snakebite mortality requires comprehensive and systemic interventions. This includes strengthening infrastructure in primary and rural healthcare centres, ensuring the widespread availability of antivenom supported by proper storage and efficient distribution systems, and training healthcare professionals in effective snakebite management and safe antivenom administration. Equally important is the implementation of community awareness programmes to promote early hospital visits and discourage delays caused by reliance on traditional or unscientific treatments.