Context:
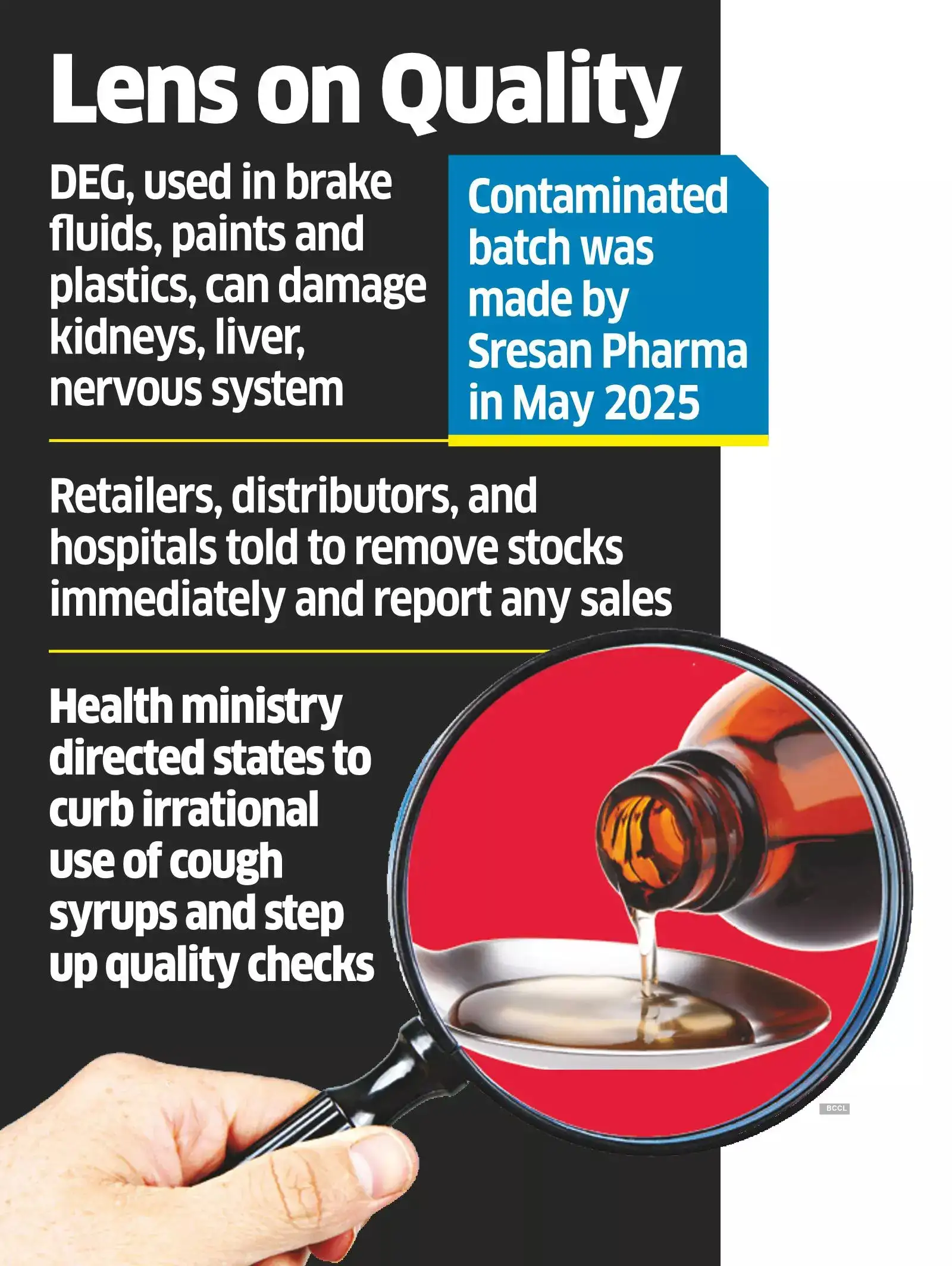
Recently, three cough syrups sold in India—ColdRif, Respifresh TR, and ReLife—were found to contain very high amounts of a toxic chemical called diethylene glycol (DEG). After testing confirmed the contamination, authorities banned these syrups and started investigations. Sadly, many children who took these syrups fell seriously ill and some even died, especially in Madhya Pradesh. After testing confirmed the contamination, authorities banned these syrups and started investigations.
About Diethylene Glycol (DEG):
-
- Diethylene glycol (DEG) is a colorless, odorless, hygroscopic organic solvent used industrially in antifreeze, brake fluids, plastics, and other applications.
- In pharmaceuticals, excipients such as glycerine or propylene glycol may inadvertently be contaminated with DEG if low-grade or industrial-grade materials are used instead of pharmaceutical-grade. Regulatory standards generally allow DEG ≤ 0.1 % in medicinal preparations — above that it is deemed unsafe.
- When people, especially children, swallow DEG, it can damage their kidneys and cause symptoms like vomiting, stomach pain, and even kidney failure. Children are more at risk because their bodies are smaller and still developing.
- Diethylene glycol (DEG) is a colorless, odorless, hygroscopic organic solvent used industrially in antifreeze, brake fluids, plastics, and other applications.
Systemic Gaps that revealed:
-
- Substandard or industrial-grade excipients (glycerine, propylene glycol) may be procured to cut costs, bypassing pharmaceutical-grade standards, thereby introducing DEG contamination.
- Disparities between regulations for domestic use and export: earlier, stricter testing was mandated for exported drugs, but domestic batches often escaped equivalent scrutiny.
- State drug control authorities may lack capacity, infrastructure, or technical competence to detect such contaminants at scale and with frequency.
- Delays or gaps in inspections, audits, lab testing, and follow‑ups allow faulty products to reach end-users.
- Substandard or industrial-grade excipients (glycerine, propylene glycol) may be procured to cut costs, bypassing pharmaceutical-grade standards, thereby introducing DEG contamination.
How drugs and cough syrups regulated in India?
-
- In India, drug manufacturing is governed by a dual regulatory system involving both central and state authorities under the Drugs and Cosmetics Act, 1940. The Central Drugs Standard Control Organisation (CDSCO), led by the Drugs Controller General of India (DCGI), oversees national-level functions such as new drug approvals, clinical trials, import controls, and setting quality standards.
- At the state level, State Drug Licensing Authorities (SLAs) manage daily enforcement, including issuing manufacturing licenses, conducting factory inspections, and investigating violations within their jurisdictions.
- Manufacturers must follow Good Manufacturing Practices (GMP) outlined in Schedule M of the Drugs and Cosmetics Rules. Licenses are issued by state drug controllers after reviewing manufacturing processes and quality systems.
- In India, drug manufacturing is governed by a dual regulatory system involving both central and state authorities under the Drugs and Cosmetics Act, 1940. The Central Drugs Standard Control Organisation (CDSCO), led by the Drugs Controller General of India (DCGI), oversees national-level functions such as new drug approvals, clinical trials, import controls, and setting quality standards.
Way Forward:
-
- Better Testing & Regulation: Test every batch of syrups for toxins; upgrade drug labs; increase surprise inspections; enforce strict quality and vendor standards.
- Legal Action & Accountability: Punish offenders severely; enforce quick product recalls; provide compensation to victims.
- Transparency & Public Awareness: Create public databases of recalled medicines; send alerts to consumers and pharmacies; educate people about safe medicine use.
- Focus on Children’s Medicines: Set higher safety standards for pediatric drugs; limit irrational cough syrup use in kids.
- Improved Coordination: Ensure central and state agencies work together; conduct regular audits; collaborate with global health bodies to track risks.
- Better Testing & Regulation: Test every batch of syrups for toxins; upgrade drug labs; increase surprise inspections; enforce strict quality and vendor standards.
Conclusion:
The discovery of three cough syrups contaminated with toxic diethylene glycol exposes serious gaps in India’s drug safety system. Beyond the immediate tragedy, it highlights flaws in raw material quality, regulation, and accountability. Protecting children’s health requires urgent reforms, strict actions, and constant vigilance to prevent such incidents from happening again.