Introduction
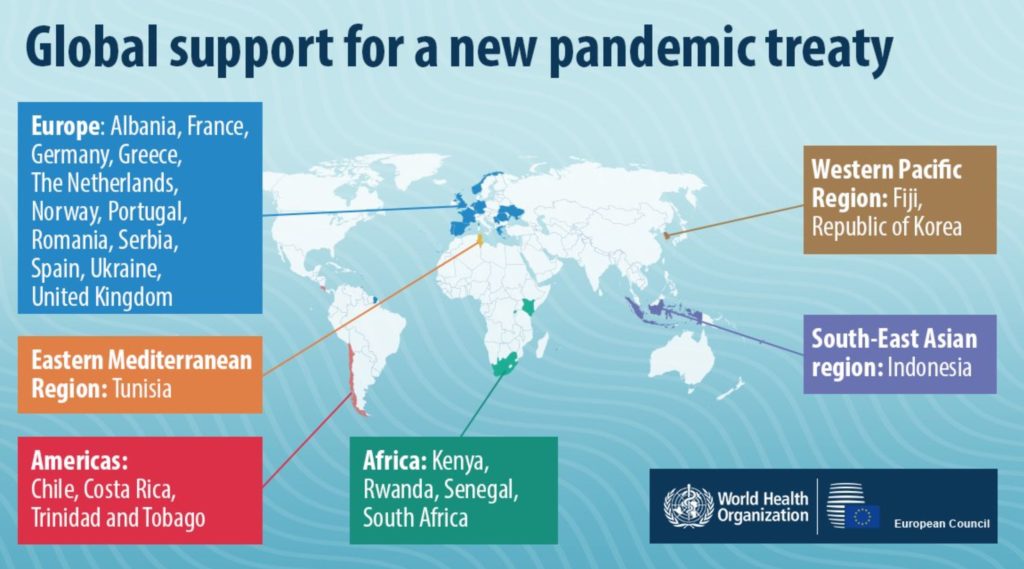
In a historic move, member states of the World Health Organization (WHO) reached consensus last week on the draft of a legally binding international treaty to enhance preparedness for future pandemics. This treaty, expected to be formally ratified at the World Health Assembly in May, marks only the second such agreement in WHO’s 75-year history—the first being the 2003 Framework Convention on Tobacco Control. Notably, the treaty has been finalized without the participation of the United States, a significant absence given its global influence in healthcare innovation and production.
Rationale behind the Pandemic Treaty
The reason behind creating the pandemic treaty came from the unfairness and confusion seen during the COVID-19 pandemic. Rich countries stored large amounts of vaccines for themselves, while there was not enough cooperation globally when the Omicron variant spread in late 2021. These issues showed serious problems in the way the world was handling health emergencies.
A 2022 Nature study estimated that over a million lives could have been saved through equitable vaccine distribution. Furthermore, the Independent Panel for Pandemic Preparedness and Response described the global response to COVID-19 as a product of “poor strategic choices” and “an uncoordinated system,” leading to an avoidable humanitarian catastrophe.
In response, WHO member states began deliberations in December 2021 to create a legally binding framework aimed at preventing similar failures during future pandemics. The agreement comes after 13 negotiation rounds spanning more than three years.
Core Provisions of the Draft Treaty
1. Pathogen Access and Benefit Sharing (PABS):
The treaty introduces a PABS system designed to facilitate the rapid sharing of pathogen samples and genetic data among nations and pharmaceutical companies. In return, it mandates a more equitable distribution of resulting vaccines, therapeutics, and diagnostics.
2. Equitable Resource Allocation:
o Participating manufacturers must allocate 10% of their output to the WHO for global distribution.
o An additional 10% must be offered at affordable rates, especially to low- and middle-income countries.
3. Technology Transfer and Local Manufacturing:
Member states are urged to promote and incentivize the transfer of technological knowledge to enhance production capacity in developing countries. This includes sharing know-how to enable the manufacture of vaccines and treatments locally.
4. Funding Conditions:
Governments are encouraged to implement policies ensuring that research funded through public money includes provisions for equitable access to the end products during pandemics. This would apply to grants made to both public institutions and private entities.
5. National Sovereignty Clause:
The treaty explicitly affirms the sovereignty of member states. Clause 24, paragraph 3, states that the treaty shall not empower the WHO Secretariat or Director-General to alter domestic laws or policies. Furthermore, WHO cannot enforce lockdowns, vaccination mandates, or travel restrictions under the treaty.
Implications of the Treaty:
The treaty's ratification by 191 countries signals a revival of multilateralism, reaffirming global trust in WHO-led health governance despite the U.S. withdrawal. It also reflects the growing bargaining power of the Global South, which successfully pushed for stronger equity-based clauses against the backdrop of a longstanding North-South divide.
While developed nations primarily emphasized access to scientific data, developing countries prioritized equitable distribution of health technologies—a compromise that now defines the treaty's character.
The treaty seeks to transform how global public health threats are detected and addressed. It:
- Establishes mechanisms for early detection and prevention of infectious diseases.
- Encourages collaborative research and international surveillance networks.
- Strengthens early warning systems through mandatory cross-border sharing of pathogen data, thereby enhancing global response readiness.
Criteria for Declaring a Pandemic Emergency
1. The event must qualify as a Public Health Emergency of International Concern (PHEIC).
2. It must constitute a public health risk to other states through international disease spread.
3. It must potentially require a coordinated international response.
4. The event must be of a communicable disease nature.
5. It must either exceed or pose a high risk of exceeding the capacity of health systems.
6. It should be causing or at high risk of causing substantial social and/or economic disruption and require rapid, equitable, and enhanced international action.
These criteria aim to clearly define situations warranting global intervention, thereby standardizing the global response mechanism.
Challenges and Limitations:
- Lack of Enforcement Mechanisms: The WHO is not granted the authority to enforce compliance with treaty provisions. This could render the agreement ineffective in crisis scenarios similar to the vaccine nationalism seen during the COVID-19 pandemic.
- Absence of the United States: The U.S., a major player in global health innovation and production, withdrew from the negotiations following President Donald Trump's return to office and his decision to exit the WHO. Experts argue that the absence of U.S. ratification significantly weakens the treaty’s global impact.
- Intellectual Property Concerns: The pharmaceutical industry has expressed apprehensions regarding the treaty’s implications for intellectual property (IP). Dr. David Reddy of the International Federation of Pharmaceutical Manufacturers and Associations emphasized that IP protection and legal certainty are vital for encouraging high-risk R&D and fostering voluntary partnerships necessary during pandemics.
- Uncertain Implementation of PABS: The operational framework for the PABS system remains vague. Clear guidelines are yet to be established for how samples and benefits will be shared and monitored during future health emergencies.
Conclusion:
The WHO pandemic treaty represents a pivotal effort to address global health inequities and improve coordination in future pandemics. By emphasizing equitable access, local manufacturing, and transparency in research funding, the treaty aims to rectify systemic failures experienced during the COVID-19 crisis. It also underscores evolving geopolitical dynamics, scientific cooperation, and normative legal principles in global health governance. However, its success will depend heavily on the political will of member states, the inclusion of influential countries like the U.S., and the creation of effective implementation and enforcement mechanisms. As the global community moves toward ratification, it remains to be seen whether this legal framework will mark a turning point in pandemic preparedness or fall short of its ambitious goals.
Main question: Discuss the significance of the WHO Pandemic Treaty as a legally binding instrument in the context of international public health governance. What does its near-universal ratification suggest about the revival of multilateralism?