Introduction:
World Heart Day is observed annually on 29 September, coordinated globally by the World Heart Federation (WHF) in collaboration with the World Health Organization (WHO) and national governments. The day serves to raise awareness on cardiovascular diseases (CVDs), which account for the largest share of global mortality.
-
- The 2025 theme, “Don’t Miss a Beat”, emphasises vigilance against silent risk factors—hypertension, diabetes, obesity, and fatty liver, which often remain undetected until complications arise.
- The recently released Apollo Health of the Nation 2025 study offers a worrying snapshot of India’s cardiovascular health. It documents an alarming rise in early-age hypertension, fatty liver disease, and hidden coronary calcium deposits among urban populations—indicating that the country is entering a “silent epidemic” phase of CVDs.
- The 2025 theme, “Don’t Miss a Beat”, emphasises vigilance against silent risk factors—hypertension, diabetes, obesity, and fatty liver, which often remain undetected until complications arise.
The Importance of World Heart Day:
Globally, CVDs are responsible for 32% of deaths (19.8 million in 2022, WHO). Of these, 85% are due to heart attacks and strokes.
In India, which houses 18% of the world’s population, the share of premature CVD mortality is disproportionately high. According to the Global Burden of Disease Study (2020):
· Nearly 28% of all deaths in India are caused by CVDs.
· 25% of heart attacks in India occur under the age of 40, compared to less than 5% in Western countries.
· By 2030, India is projected to lose $237 billion in economic output due to premature CVD deaths (World Economic Forum estimate).
Thus, World Heart Day assumes particular importance for India—not just as a health campaign, but as a developmental imperative.
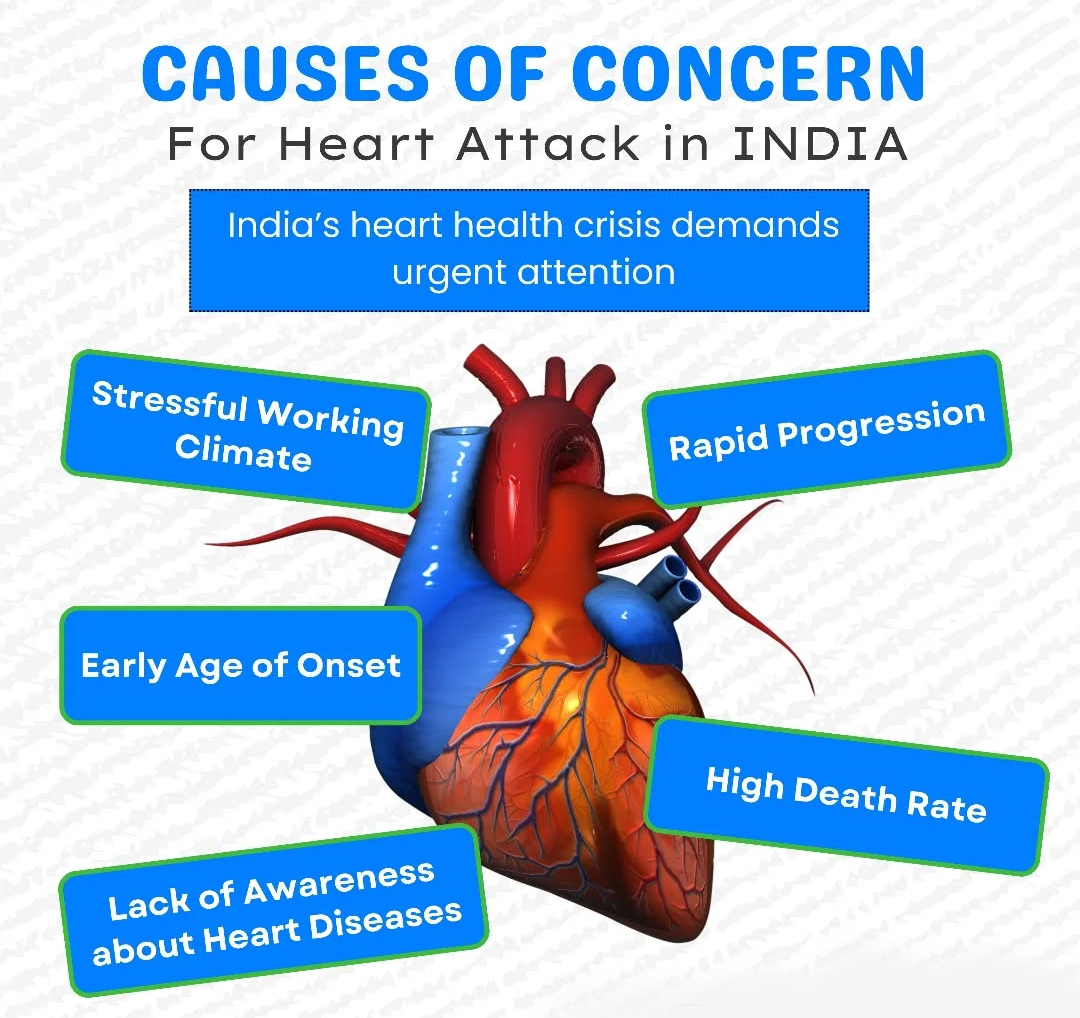
Why Cardiovascular Diseases Matter in India?
The drivers of CVDs in India are multi-dimensional:
1. Genetic Susceptibility
o South Asians develop CVDs 5–10 years earlier than Western populations.
o Indians are prone to “thin-fat” phenotype—normal weight but high visceral fat, insulin resistance, and higher lipoprotein (a) levels.
2. Nutrition Transition
o NFHS-5 shows rising obesity: 24% women and 23% men in urban India are overweight/obese.
o India consumes 10.9 g of salt per day, double the WHO recommended limit (5 g/day).
o Trans fats, though restricted, persist in fried street foods and packaged snacks.
3. Physical Inactivity
o The ICMR-INDIAB study (2022) found that nearly 40% of Indians are inactive, with women and urban populations at greater risk.
4. Environmental Stressors
o According to Lancet Planetary Health (2022), air pollution contributed to 1.67 million deaths in India in 2019, of which over half were CVD-related.
o Chronic stress and irregular sleep cycles, especially in urban work culture, aggravate hypertension and metabolic disorders.
o This convergence of risks makes India the epicentre of the global CVD crisis.
Key Findings from Apollo’s Health of the Nation 2025 Study:
The study highlights regional variations in hidden risks:
-
-
- Delhi-NCR: Hypertension rates rising; 65% had fatty liver, linked to lifestyle and pollution.
- Mumbai: 46% of asymptomatic individuals had coronary calcium deposits; 25% obstructive CAD; 2.5% below 40 years.
- Chennai: Diabetes prevalence at 29% and pre-diabetes at 37%.
- Bengaluru: Sedentary IT workforce with early hypertension and dyslipidemia.
- Hyderabad: Over 80% of fatty liver patients were diabetic; 75% hypertensives also had fatty liver.
- Kolkata: Dual burden of hypertension/diabetes alongside anemia and micronutrient deficiencies.
- Lucknow (Tier 2): College students showed 28% overweight and 19% pre-hypertensive rates.
- Delhi-NCR: Hypertension rates rising; 65% had fatty liver, linked to lifestyle and pollution.
-
This evidence confirms that India’s CVD burden is not limited to metros or the elderly but is pervasive across age groups and geographies.
The Emergency Preparedness Gap in India:
-
- Incidence: About 600,000 out-of-hospital cardiac arrests annually (40 per 100,000).
- Survival: Less than 5%, compared to 10–20% in developed nations.
- Gaps:
- Low public awareness of CPR.
- Scarcity of AEDs in public spaces.
- Limited access to implantable cardioverter-defibrillators (ICDs).
- Low public awareness of CPR.
- Incidence: About 600,000 out-of-hospital cardiac arrests annually (40 per 100,000).
Global best practice: Countries like Japan and the US have universal CPR training in schools, mandatory AEDs in public areas, and national emergency response networks—models India can adapt.
Common Symptoms of Cardiovascular Disease:
-
- Heart Attack: Chest pain, breathlessness, cold sweats, pain radiating to jaw/arm.
- Stroke: FAST symptoms (Face drooping, Arm weakness, Speech difficulty, Time to call help).
- Rheumatic Heart Disease: Fatigue, irregular heartbeats, chest discomfort—often linked to untreated sore throat in childhood.
- Heart Attack: Chest pain, breathlessness, cold sweats, pain radiating to jaw/arm.
Why CVDs Are a Development Challenge
-
- Global dimension: 80% of CVD deaths occur in low- and middle-income countries (LMICs).
- India-specific:
- Economic loss: $2.17 trillion projected loss (2012–2030) due to NCDs (World Economic Forum).
- Health inequality: Rural India lacks diagnostic facilities—hypertension control rate is only 15% (Lancet, 2019).
- Social burden: Catastrophic out-of-pocket expenditure; NFHS-5 shows 55% of health expenses are borne by households.
- Economic loss: $2.17 trillion projected loss (2012–2030) due to NCDs (World Economic Forum).
- Global dimension: 80% of CVD deaths occur in low- and middle-income countries (LMICs).
Policy Priorities for India:
1. Prevention-first healthcare
o WHO’s “Best Buys”: Eliminate trans fats, cut salt by 30%, and reduce tobacco use.
o India’s action: Trans fats phased out by 2022; Fit India Movement promotes activity; Eat Right India campaign encourages healthier diets.
2. Strengthening Primary Healthcare
o Ayushman Bharat Health and Wellness Centres (HWCs) include screening for hypertension, diabetes, and common NCDs.
o NP-NCD (National Programme for Prevention & Control of Non-Communicable Diseases, 2023) mainstreams NCD care into primary health services.
3. Emergency Preparedness
o National guidelines needed for AED deployment and CPR training.
o Integration with 108 ambulance services and AI-based triage in metros.
4. Community and Workplace Health
o Periodic health check-ups, wellness leave, and workplace fitness programmes.
5. Research and Indigenous Data
o Expansion of the ICMR-NCDIR (National Centre for Disease Informatics and Research) for robust surveillance.
o Promotion of India-specific trials on lipoprotein (a) and genetic predispositions.
6. Global Partnerships
o Align with WHO Global HEARTS Initiative and UN SDG 3.4 target: reduce premature mortality from NCDs by one-third by 2030.
Conclusion:
World Heart Day 2025 reminds us that cardiovascular diseases are no longer just a health challenge but a developmental imperative for India. With rising premature mortality, economic losses, and widening health inequalities, the fight against CVDs requires a prevention-first approach, stronger primary healthcare, and robust emergency preparedness. Aligning national efforts with global best practices and SDG targets will be crucial to safeguard India’s demographic dividend and ensure that the nation does not “miss a beat” in securing its collective health.
| UPSC/PSC Main Question: Cardiovascular diseases (CVDs) have emerged as India’s “silent epidemic.” Discuss the policy challenges in addressing this growing crisis. |