Context:
Happiness alone is not a sign of good mental health, it includes emotional, social, cognitive, and physical balance that enables people to handle life’s challenges effectively. In recent years, especially after the COVID-19 pandemic, global awareness and dialogue around mental health as a fundamental human right have grown significantly.
-
- This reality was starkly reflected in the data shared during a national mental health conference in Bengaluru, revealing that India’s national mental health helpline, Tele-Manas, has received over 25 lakh calls since its launch in October 2022. Among them, more than 39,000 were suicide-related distress calls, underscoring both the scale of emotional suffering and the growing public trust in accessible tele-mental health services.
- In just three years, the helpline has emerged as a vital support system - with nearly 7,700 calls escalated for advanced counselling, and over 5,800 cases identified as acute emergencies. States such as Tamil Nadu, Maharashtra, Karnataka, and Uttar Pradesh have recorded the highest call volumes, while the majority of callers are between 18 and 45 years old - the country’s most productive age group.
- This reality was starkly reflected in the data shared during a national mental health conference in Bengaluru, revealing that India’s national mental health helpline, Tele-Manas, has received over 25 lakh calls since its launch in October 2022. Among them, more than 39,000 were suicide-related distress calls, underscoring both the scale of emotional suffering and the growing public trust in accessible tele-mental health services.
The State of Mental Health in India:
-
- Mental health disorders are now among the leading causes of disability worldwide, and India carries a significant share of this burden. According to the National Mental Health Survey (2015–16) conducted by NIMHANS, nearly 11% of Indian adults live with a diagnosable mental disorder. Around 15% of adults require mental health intervention, while 13.7% have experienced mental illness at some point in their lives.
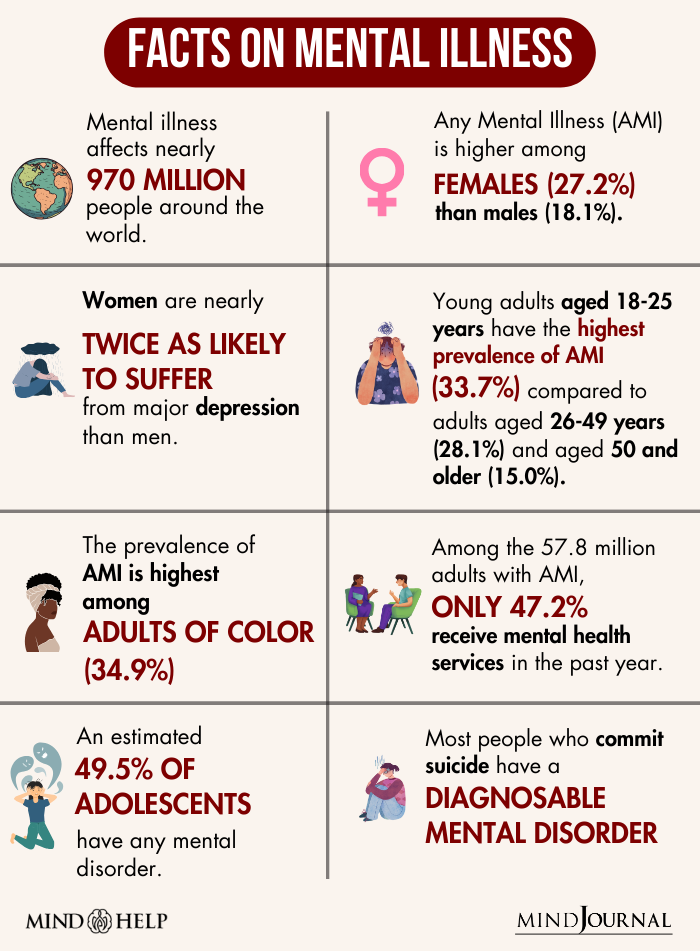
- Urban India reports higher prevalence rates than rural areas, largely due to stress, social isolation, and changing lifestyles. Notably, women are twice as likely as men to experience mental health disorders such as depression and anxiety.
- Mental health disorders are now among the leading causes of disability worldwide, and India carries a significant share of this burden. According to the National Mental Health Survey (2015–16) conducted by NIMHANS, nearly 11% of Indian adults live with a diagnosable mental disorder. Around 15% of adults require mental health intervention, while 13.7% have experienced mental illness at some point in their lives.
Rising Suicide Rates:
India’s suicide rate has been rising steadily. As per the NCRB’s 2023 report, the country recorded 1,71,418 suicides, with males accounting for nearly 73% of the total. Economic distress, social isolation, discrimination, academic pressure, and relationship issues continue to drive many towards despair. The data from Tele-Manas highlights the urgency of expanding community-based mental health care and preventive support.
Understanding the Treatment Gap:
-
- Despite increasing awareness, India faces a massive treatment gap—between 70% and 92% of people with mental disorders do not receive adequate care. The shortage of professionals is a key factor: while the WHO recommends three psychiatrists per 100,000 people, India has only 0.75 psychiatrists per 100,000.
- Social stigma, limited infrastructure, and lack of awareness further deter people from seeking help. Many continue to suffer silently due to fears of being judged, discriminated against, or labelled as “weak” or “unstable”.
- Despite increasing awareness, India faces a massive treatment gap—between 70% and 92% of people with mental disorders do not receive adequate care. The shortage of professionals is a key factor: while the WHO recommends three psychiatrists per 100,000 people, India has only 0.75 psychiatrists per 100,000.
Impact of Poor Mental Health:
-
- Health Consequences: Mental and physical health are deeply interconnected. Individuals suffering from depression or anxiety are more vulnerable to chronic illnesses such as cardiovascular diseases, diabetes, and sleep disorders. A Lancet Psychiatry (2025) study revealed that people with depression have a 72% higher risk of developing heart disease.
- Economic Costs: Poor mental health directly impacts productivity, employability, and income levels. According to WHO estimates, depression and anxiety cost the global economy US$1 trillion annually in lost productivity. By 2030, the total financial burden of mental health conditions is projected to reach US$16 trillion globally. In India, workplace stress and burnout are emerging as major challenges, especially among the youth.
- Social and Relationship Strain: People with mental health disorders often face social isolation and strained family relations. This lack of social support not only worsens symptoms but also reduces the chances of recovery.
- Stigma and Discrimination: The stigma surrounding mental illness remains a major barrier. It manifests in shame, exclusion, and institutional neglect. Studies show that stigma is especially severe in low- and middle-income countries, including India, where mental illness is often misunderstood as a personal weakness rather than a medical condition.
- Health Consequences: Mental and physical health are deeply interconnected. Individuals suffering from depression or anxiety are more vulnerable to chronic illnesses such as cardiovascular diseases, diabetes, and sleep disorders. A Lancet Psychiatry (2025) study revealed that people with depression have a 72% higher risk of developing heart disease.
Youth and the Mental Health Crisis:
-
- Half of all mental health conditions begin by the age of 14, and three-fourths by the mid-twenties. Young people today face enormous academic, social, and digital pressures. Exposure to online content related to suicide and self-harm, along with cyberbullying and social isolation, has worsened mental distress among adolescents.
- Experts have repeatedly warned that ignoring mental health at this stage can have lifelong consequences — from poor academic outcomes to higher substance use and self-harm tendencies.
- Half of all mental health conditions begin by the age of 14, and three-fourths by the mid-twenties. Young people today face enormous academic, social, and digital pressures. Exposure to online content related to suicide and self-harm, along with cyberbullying and social isolation, has worsened mental distress among adolescents.
Global Policy Frameworks:
The WHO’s Comprehensive Mental Health Action Plan (2013–2030) provides a roadmap for member countries to strengthen leadership, community care, and mental health promotion. The 2022 World Mental Health Report calls for transformative actions through three pathways:
-
- Deepening Value and Commitment – Recognising mental health as integral to overall well-being.
- Reshaping Environments – Improving social, physical, and economic settings to promote mental wellness.
- Strengthening Care Systems – Shifting from institutional care to community-based, integrated models.
- Deepening Value and Commitment – Recognising mental health as integral to overall well-being.
WHO also advocates for integrating mental health services into Universal Health Coverage (UHC) ensuring access, affordability, and dignity for all.
India’s Comprehensive Push for Mental Health:
-
- National Mental Health Programme (NMHP): Launched in 1982, NMHP aims to integrate mental healthcare into the general health system and make services accessible to all. Its District Mental Health Programme (DMHP), launched in 1996, now covers 767 districts, offering counselling, inpatient care, suicide prevention, and awareness campaigns.
- National Suicide Prevention Strategy (2022): India’s first dedicated National Suicide Prevention Strategy (NSPS) aims to reduce suicide mortality by 10% by 2030. It focuses on mental health screenings in schools and workplaces, crisis helplines, and targeted interventions for high-risk groups such as students, farmers, and young adults.
- Strengthening Manpower and Infrastructure: India has 47 government-run mental hospitals and 25 Centres of Excellence for advanced psychiatric education and research. The Digital Academies established at NIMHANS, LGBRIMH, and CIP Ranchi have trained over 1.7 lakh health professionals in mental health management and counselling.
- Digital and Community-Based Interventions: The Tele-Manas platform, launched in 2022, offers 24x7 tele-counselling in multiple languages. Integrated into the Ayushman Bharat initiative, it connects callers to trained counsellors and psychiatrists and provides escalation support for high-risk cases. The initiative has been endorsed by the WHO as a model for community-based mental healthcare.
- Ayushman Bharat and Mental Health Integration: Mental health has now been integrated into Ayushman Arogya Mandirs — upgraded primary health centres that deliver comprehensive care. Under PM-JAY, mental disorders are covered under a ₹5 lakh insurance plan per family, with over 1.35 lakh admissions already authorised for psychiatric care.
- National Mental Health Programme (NMHP): Launched in 1982, NMHP aims to integrate mental healthcare into the general health system and make services accessible to all. Its District Mental Health Programme (DMHP), launched in 1996, now covers 767 districts, offering counselling, inpatient care, suicide prevention, and awareness campaigns.
Policy Emphasis and Economic Survey 2024–25:
The Economic Survey 2024–25 stressed that India’s demographic dividend depends not just on education and physical health but also on mental well-being. It recommended:
-
- Strengthening mental health education in schools
- Expanding workplace wellness programmes
- Scaling up digital mental health initiatives like Tele-Manas
- Encouraging community participation in awareness campaigns
- Strengthening mental health education in schools
Conclusion:
India's growing mental health challenge is no longer an invisible crisis. It is a public health priority that impacts the nation's social and economic structure. While progress has been made through national programs, suicide prevention strategies, and integration into the primary health system, there is still a need for greater investment, stigma-reduction, and multi-sectoral collaboration.
| UPSC/PCS Main Question: “The real barrier to mental healthcare in India is not lack of resources, but lack of understanding.” Critically comment. |