Antimicrobial Resistance (AMR) has emerged as a global public health crisis, undermining decades of progress in infectious disease control. Characterized by the ability of microorganisms to resist the effects of antimicrobial agents, AMR has already contributed to over a million deaths globally, with India bearing a significant portion of this burden. Despite efforts at both national and global levels, India faces unique challenges stemming from healthcare infrastructure gaps, irrational use of antibiotics, and regulatory inefficiencies.
What is AMR?
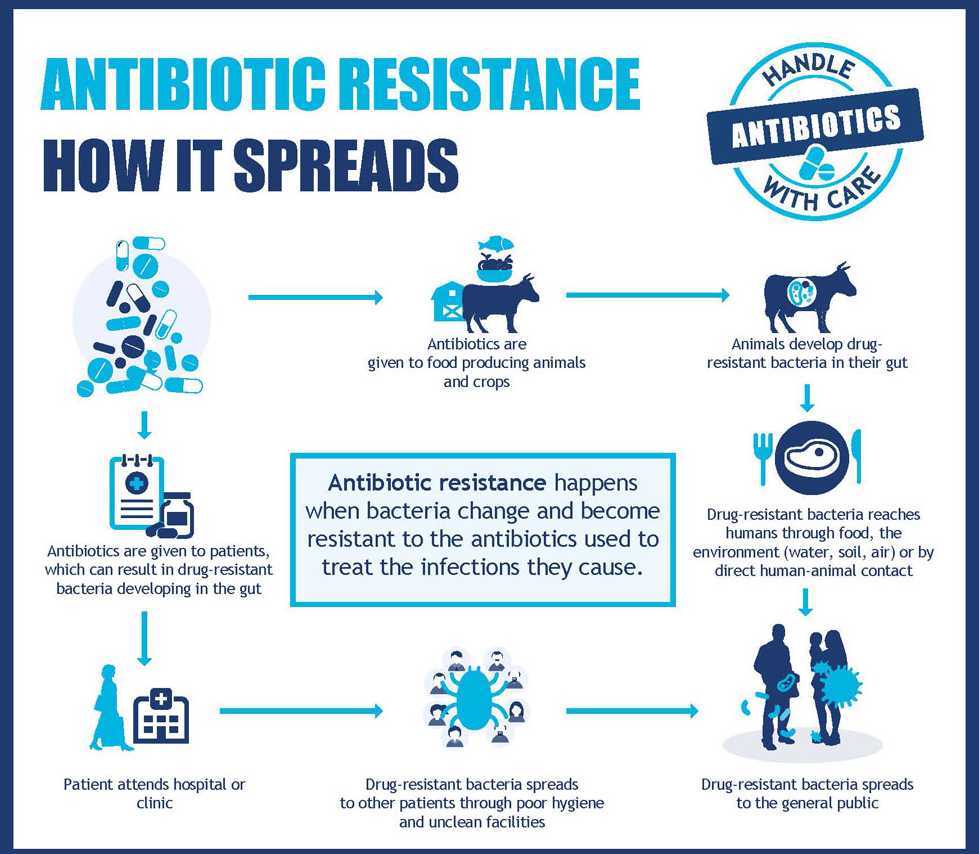
Antimicrobial resistance occurs when pathogens such as bacteria, viruses, fungi, and parasites develop the ability to withstand drugs—particularly antibiotics—that once effectively eliminated them. AMR is already contributing significantly to global mortality. According to the Institute for Health Metrics and Evaluation (IHME) at the University of Washington, 1.27 million deaths globally in 2019 were directly caused by bacterial AMR. In India alone, 2,97,000 deaths were linked to AMR, making it one of the worst-affected countries.
A 2022 study published in The Lancet projected that by 2050, AMR could cause:
· 1.91 million direct deaths annually worldwide.
· 8.22 million deaths associated with resistant infections.
The Global Health and Economic Threat:
According to the World Health Organization (WHO), AMR is among the top 10 global public health threats. Without urgent action, we may reach a point where routine surgeries, cancer treatments, and even small cuts or infections become dangerous again.
The economic toll could be devastating:
· The World Bank estimates AMR could cost an additional $1 trillion in healthcare expenses by 2050.
· Between now and 2030, global GDP losses could reach $1–3.4 trillion per year, hitting low- and middle-income countries the hardest.
· The World Organisation for Animal Health (WOAH) warns that AMR could endanger the food security of two billion people and cause up to $100 trillion in losses by 2050.
Key Drivers of AMR in India:
The rise of AMR in India is driven by both medical and non-medical factors:
1. Overuse and Misuse of Antibiotics: Only 30% of all antibiotics produced globally are used for humans.The remaining 70% are used in livestock, poultry, aquaculture, and agriculture, often as growth promoters. Even new antibiotics face premature resistance due to irrational usage.
· Experts have flagged emerging resistance to ceftazidime-avibactam, a potent newer molecule, because of overuse and lack of stewardship.
2. Over-the-Counter Sales: Despite laws requiring prescriptions for antibiotics, enforcement is weak. Pharmacies routinely sell antibiotics without medical oversight.
3. Self-Medication and Misdiagnosis: People often consume antibiotics for viral infections (e.g., flu), against which these drugs are ineffective. Diagnostic delays or errors lead to indiscriminate use of broad-spectrum antibiotics.
4. Weak Regulatory Oversight: Limited control over antibiotic marketing and distribution and insufficient surveillance of resistant pathogens, especially in rural or informal healthcare settings also impact the rise of AMR.
5. Hospital-Acquired Infections: Inadequate hygiene protocols in hospitals lead to resistant infections, especially in ICUs and post-operative wards.
A notable intervention was India’s ban on colistin as a growth promoter in poultry — a move that has helped reduce the emergence of colistin-resistant strains.
Trends in Antimicrobial Use in Animals:
Decline in Antimicrobial Use (2020–2022)
· Global antimicrobial use in animals fell by 5% during this period.
· The most significant reductions were observed in:
o Europe: 23% decline
o Africa: 20% decline
These declines indicate growing awareness and improved regulatory control in certain regions, though global disparities persist.
Use in Aquaculture and Terrestrial Animals:
· Fluoroquinolones accounted for 15.8% of all antimicrobials used in aquaculture.
· This is particularly concerning given fluoroquinolones are considered critically important antibiotics in human medicine, raising the risk of cross-resistance from aquatic to human pathogens.
Growth Promotion Practices:
· ~20% of WOAH member countries reported the use of antimicrobials as growth promoters, despite WHO and WOAH recommendations against the practice.
· Of these, 7% used highest-priority critically important antimicrobials (HP-CIAs) such as:
o Colistin
o Enrofloxacin
o Fosfomycin
The use of HP-CIAs in livestock not only compromises human medicine but also accelerates the global AMR crisis.
Why Antibiotic Innovation Has Slowed:
Despite the urgent need, few pharmaceutical companies invest in antibiotic development. The reasons are structural and financial:
· Low Profit Margins: Unlike drugs for chronic conditions, antibiotics are taken for short durations and often reserved as a last resort.
· Antibiotic Innovation Gap: Most large pharma firms have exited this space, leaving innovation to small and mid-sized firms like Wockhardt, Orchid Pharma, and Bugworks.
· Regulatory Challenges: Lengthy approval timelines and lack of regulatory incentives discourage investment.
· Affordability Concerns: Wockhardt plans to use tiered pricing, offering drugs at up to 80% lower cost in India compared to Western markets to improve accessibility.
India’s key initiatives to combat Antimicrobial Resistance (AMR):
· National Programme on AMR Containment (2012–17):
o Established lab-based AMR surveillance
o Promoted rational antimicrobial use and infection control
· National Action Plan on AMR (2017):
o Adopted a One Health approach involving human, animal, and environmental health sectors
· ICMR’s AMR Surveillance and Research Network (AMRSN, 2013):
o Tracks resistance patterns across India
o Provides data for policy and clinical decision-making
· Research and International Collaboration:
o Focused on new drug development and capacity building
· AI in the Fight Against AMR
o AMRSense: An AI-powered tool that uses hospital data to predict antibiotic resistance trends
o AMROrbit Scorecard: Visual tool to help hospitals track resistance patterns which compares local resistance rates with global averages and flags high-risk areas for timely intervention
Conclusion:
AMR is not a distant or future threat; it is a current and accelerating crisis. It affects individuals and families, healthcare systems, economies, and global development. Scientific innovations offer hope — but only if they are protected by strong stewardship, regulatory reform, and public education.
The fight against AMR requires a multi-sectoral, coordinated approach:
· Regulate and monitor antibiotic usage across all sectors.
· Strengthen diagnostic and laboratory systems.
· Invest in public health infrastructure and training.
· Promote innovation while ensuring affordability and access.
Additionally, Experts widely agree that public awareness is one of the weakest links in the fight against AMR. Misconceptions — such as the belief that antibiotics can treat any infection — are common. Without behavioral change, even the best policies and drugs may fail. We need to be multiple steps ahead of pathogens. Otherwise, we are fighting a battle we are going to lose.
| Main question: What are the economic and public health implications of Antimicrobial Resistance (AMR) in India? Discuss the structural challenges that hinder antibiotic innovation and how India can balance access with stewardship. |